What is a gastric band?
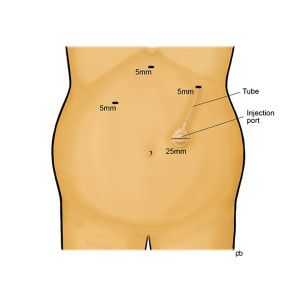
The gastric band operation is done by laparoscopy under general anaesthesia in Leeds. 4-5 small cuts are made on your abdomen (tummy). The operation takes 45 minutes to 1 hour.
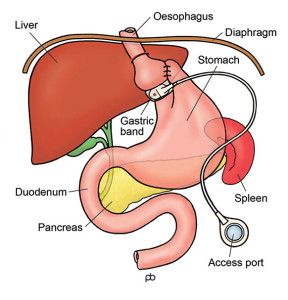
The band has three parts. There is the actual band – the belt or collar that goes around your stomach, just below where your oesophagus (gullet) joins your stomach. The band is made of a special plastic called silicone. During the operation, a special tube (called a bougie) is passed into your stomach from your mouth. This tube has a balloon at its tip and the balloon helps to place the band in the correct position. The stomach is stitched around the band in order to hold the band in place. The band is connected by a tube to small hollow disc, called the injection port. The port is fixed to the muscles of your abdominal (tummy) wall, below the skin. You cannot see the port but you might be able to feel it if you press hard. Sterile liquid can be put into and taken out from the port with a needle. It is very much like having an injection. The liquid in the port passes through the tubing to the band, which expands and compresses your stomach.
How does the gastric band work?
The band is like a tyre. It can be inflated or deflated by putting in or taking out liquid from the injection port. When the band is inflated, it will compress the walls of your stomach. Compression of the stomach wall reduces hunger and makes you feel full quickly after eating a small meal. It is believed that compression stimulates nerve endings in the stomach wall and creates signals of less hunger and more fullness. The aim is make you feel full after a small, healthy meal and not feel hungry until your next mealtime.
What is band-adjustment?
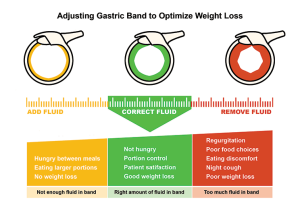
There is no liquid (or only a very small amount of liquid) in the band immediately after the operation. The band is kept empty intentionally so that it can settle into position. The first filling of the band is done about 4-6 weeks after the operation, usually (but not always) under x-ray control. You will be asked to drink a dye called barium so that compression of the stomach can be seen whilst filling the band. Most people will need 2-4 band fills to get a good sense of restriction of hunger and fullness. After the first x-ray guided band-fill, subsequent band-fills are done in the outpatient clinic. A barium swallow x-ray may be used again if your progress is not as expected. Sometimes the band may become too tight after a fill, and some liquid may need to be taken out. There is some trial and error in band-adjustment. You can think of it as fine-tuning of the band. After each band-fill, you should take only soft food for 2-3 days and then gradually build up to normal food. It is best to leave 2-4 weeks between band-fills.
How will I know when my band is properly adjusted?
The aim is for you to get a feeling of fullness quickly after eating, so that you can control your portion-sizes. Also, your appetite should be controlled so that you do not feel hungry between mealtimes. But, the band should not be over-filled. If the band is too tight, you can get difficulty to swallow, regurgitation and heartburn. Liquid will need to be taken out from the band. The idea is for you to feel satisfied with small, healthy meals. This is called the green zone of the band. Mr Sarela and the specialist dietician will guide you through this process.
Will I need any more band-fills after the band has been adjusted?
As you lose weight, there can be some increase or decrease in the sense of restriction from the band. There can be loss of very small amounts of liquids from the band over time and top-ups may be needed. Some people increase their physical activity to a level where they need extra nutrition and want less restriction. The band is a life-long tool for weight control. Periodic maintenance will be needed.
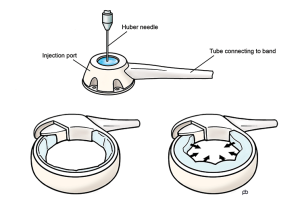
Is there special equipment for band adjustment?
It is very important to use a special needle called the Huber needle. The injection port of the band has a membrane that allows the needle to enter into the port. An ordinary injection needle can tear this membrane and allow the liquid to leak out. If this happens, the band stops working and an operation will be needed to change the port. The Huber needle has a special type of tip – called a non-coring tip – that does not damage the membrane.
Is the gastric band a reversible procedure?
Yes, the band is reversible in the sense that it can be taken out. But, you should not think of the band as temporary treatment. The purpose of the band is to help you to lose weight. Once you have lost weight, the band then helps you to maintain your weight. It is very likely that you will put weight back on if the band is taken out. The band is taken out only if it has caused some problem or complication.
How much weight can I lose with a gastric band?
Your weight loss will depend on your starting BMI and gender. Please remember that there are no guarantees in weight loss surgery.
If you are a woman and your starting BMI is less than 50, you could lose about 55-60% of your excess weight (%EWL). If your BMI is more than 50, the average weight loss is lower: about 40% EWL.
If you are a man and your BMI is less than 50, you could have 45-50%EWL . If your BMI is more than 50, the average weight loss is lower: about 40%EWL.
You will lose weight over 2-3 years after the operation. After this time, weight-loss stops and you have reached your new weight. This new weight is called the plateau. You could imagine that the gastric band has reset a weigh-thermostat in your body. The gastric band helps you to maintain your new weight once you have reached your plateau.
What is the follow-up for a gastric band?
Apart from band-adjustment, lifelong medical follow-up is essential. This can be done with your GP. A detailed discharge summary will be sent to your GP, explaining the follow-up. Please make an appointment to see your GP soon after your operation. You can think of the follow-up care in 3 parts: