Click images for a larger version and full description
I have been diagnosed with cancer of the oesophagus. What should I do next?
Oesophagus cancer is diagnosed by endoscopy. The diagnosis of cancer is confirmed by laboratory examination of biopsies taken at endoscopy. You should urgently see a specialist once you have been diagnosed with cancer of the oesophagus. NHS hospitals in the UK have a system by which all patients with oesophagus cancer are cared for by a specialist multi-disciplinary team (MDT). The entire MDT will discuss your case at their regular meetings and will remain involved throughout your treatment. Most private hospitals in the UK will not have an oesophagus cancer MDT. If you are having treatment in a private hospital, your case will be discussed by the MDT in the local NHS hospital. For example, if you see Mr Sarela at the Nuffield Hospital Leeds or the Spire Hospital Leeds, he will discuss your case in the MDT meeting at St James’s University Hospital.
How can I understand the stage of the cancer of my oesophagus?
The stage of the cancer depends on three parts. First, how deep does the tumour penetrate into the wall of the oesophagus? This is called the ‘T’ stage of the cancer. The T stage can be T1, T2, T3 or T4. The numbering indicates the layer of the oesophagus wall that is involved by the cancer. A T1 cancer involves only the innermost layers, called the mucosa and sub-mucosa. If the tumour extends into the muscle layer, it is called T2. If it goes further into the outermost lining of the oesophagus, called the adventitia, it is T3. The tumour is T4 if it goes into another structure, like the aorta or spine that lie next to the oesophagus.
The second part of staging is about spread of the cancer to the lymph glands that lie next to the oesophagus. This is called the ‘N’ stage of the cancer. The stage is N0 is no lymph glands are involved by cancer. When there is spread to lymph glands, the stage may be N1 or N2 depending on the number of glands that is involved.
The third part of staging is to find out if the cancer has spread outside the oesophagus and the nearby lymph glands. Such distant spread is called metastasis. Common places for spread of oesophagus cancer are the liver, lungs, bones and lymph glands far from oesophagus. The stage is M0 if there is no sign of spread. If the cancer has spread, the stage is M1.
These three parts together make up the TNM stage of cancer. For example, the tumour may be in the muscle layer of the oesophagus (T2) with no spread to lymph glands (N0) or to distant sites (M0). The TNM stage is expressed as T2N0M0. The cancer stage can be stated as 1, 2, 3 or 4 based on different combination of T and N and M. But, it is more useful to think and talk in terms of TNM for planning treatment.
Also, it is important to remember that staging depends on tests. Soon after the diagnosis, staging is done by scans and other tests. This is called radiological or clinical staging. If an operation is done at a later stage, then the tumour will be examined the pathology laboratory and a pathological stage will be given. The planning of treatment is done usually on the basis of the clinical stage because the pathological stage comes to light only later. The pathological stage can be different from the clinical stage because x-rays and scans cannot match the accuracy of pathology.
What tests will I need to have to find out the stage of the cancer of my oesophagus?
It is very important to find out the stage of the cancer because treatment depends on the stage. The first staging test is a CT scan. The main purpose of the CT scan is to find out if your cancer has spread outside the oesophagus. Also, the CT scan can give valuable information about the location of the tumour in your oesophagus, the size of the tumour and the depth of penetration into the wall of your oesophagus.
If the CT scan unfortunately shows that your cancer has spread to a distant area, like the liver or lungs, no more staging tests are needed. If the CT scan does not show any distant spread, the next test usually is a PET scan. PET is a special type of scan that checks for metabolic activity in tumours. The reason for doing a PET is that CT scan does not always pick up distant spread. PET scanning improves the accuracy of staging. If both CT and PET are negative for distant spread, an EUS test may be done next. EUS (Endoscopic UltraSound) is a special type of endoscopy where an ultrasound scan is done from the inside of your oesophagus. This can give detailed information about the depth of the tumour and involvement of lymph glands. You may need to have a diagnostic laparoscopy. The inside of the tummy is directly examined, and biopsies may be taken.
The information from all these tests is put together to make up the clinical stage of the cancer. The decision about how to treat the cancer is made on the basis of this overall clinical stage.
What are the types of cancer of the oesophagus?
There are two main types of cancer of the oesophagus: squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma (SCC) arises from the skin-like squamous cells that normally line the oesophagus. SCC is seen usually in the upper and middle parts of the oesophagus. SCC makes up about one quarter of all cancers of the oesophagus. The second type of cancer, called adenocarcinoma, develops in the lower part of the oesophagus. Usually, adenocarcinomas arise in the area where the oesophagus joins the stomach. This area is called the Gastro-Oesophageal Junction (GOJ). A cancer in this area may be called a GOJ cancer. Adenocarcinomas arise from gland-like cells, called Barrett’s oesophagus. These Barrett’s cells develop because of damage to the original squamous cells by acid reflux. Adenocarcinomas make up more than half of all cancers of the oesophagus. Sometimes, the pathologist may not be able to tell the difference between SCC and adenocarcinoma. In such cases, the cancer is said to be undifferentiated. There are some other rare types of oesophageal cancer called small cell carcinoma and neuroendocrine carcinoma.
Do I need an operation to treat the cancer of my oesophagus?
The decision about whether to do an operation for cancer of the oesophagus depends on two important factors. First, what is the stage of the cancer? And second, what is your general medical condition and fitness? Cancer of the oesophagus can be cured by an operation to remove the oesophagus and adjacent lymph glands. But, this is very major surgery and the decision should be made with great care.
Broadly, there are three situations where an operation is not done:
1) An operation will not help if the cancer has spread (stage M1). You will be referred to see an oncologist to discuss chemotherapy.
2) Even if the cancer is at a curable stage (stage M0), a careful assessment has to be made of the risks of the operation for you, based on your individual fitness and medical problems. The fitness of your heart and lungs is checked by a cardiopulmonary exercise (CPX) test. You will be asked to pedal on a special exercise bicycle, with monitoring of your heart and lungs. If the risk of life-threatening complications seems too high, then non-surgical alternatives should be explored. Ultimately, the decision has to be tailor-made for you. If an operation is not felt to be suitable, you can see an oncologist to discuss chemotherapy and radiotherapy.
3) An operation may not be needed if the cancer involves only the inner most layers of the wall of the oesophagus (stage T1). It may be possible to cut out the cancer by endoscopy. This is called EMR (Endoscopic Mucosal Resection). The cut out cancer is examined in the pathology laboratory. An operation may be recommended after EMR if it appears that the cancer has not been removed completely.
What are the alternatives to an operation for treatment of cancer of the oesophagus?
If you have squamous cell carcinoma (SCC) of the oesophagus, a combination of chemotherapy and radiotherapy is an alternative to surgery. SCC can be cured by chemotherapy and radiotherapy. Surgery seems to be more effective than chemo-radiotherapy but the risks of surgery are high. You need to carefully balance the pros and cons. If you have SCC, it may be a good idea to meet both a surgeon and a clinical oncologist before making a decision about the type of treatment. Chemotherapy and radiotherapy seem to be less effective for adenocarcinoma than for SCC.
If I have an operation, will I need chemotherapy and radiotherapy also?
An operation alone may not be enough to cure cancer of the oesophagus. The tumour in the oesophagus and the surrounding lymph glands are taken out by the operation. But, there is risk that that cancer cells have spread already to other areas. The spread is microscopic and cannot be picked up by the staging tests or by inspection during the operation. These cells can grow after the operation and cause the cancer to come back (called recurrence of cancer). The risk of recurrence can be estimated by the pre-operative staging tests. For example, the risk is increased if the cancer has penetrated all the layers in the wall of the oesophagus, or if lymph nodes alongside the oesophagus are involved. Chemotherapy is usually given before the operation to bring down the risk of recurrence. Many studies have shown that it is better to give chemotherapy upfront, before the operation, rather than to wait until after the operation. Some patients may benefit from both chemotherapy and radiotherapy before surgery. In few cases, chemotherapy or radiotherapy treatment may be given after the operation. You will be referred to an oncologist to discuss chemotherapy and radiotherapy.
What is the operation for cancer of the oesophagus?
There are two types of operations for cancer of the oesophagus. One is called the Ivor Lewis (right thoraco-abdominal) operation and the other is called the McKeown (3-stage) operation.
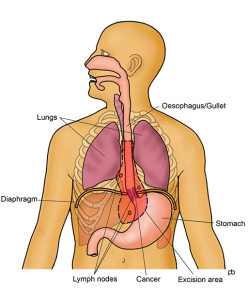
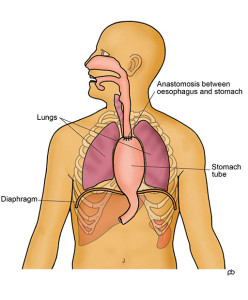
The Ivor Lewis operation is done for tumours in the lower part of the oesophagus and at the junction of the oesophagus with the stomach (the GOJ). About two-thirds of your oesophagus and a part of your stomach are removed. It is not enough to remove only the tumour because cancer cells can have spread in the wall of your oesophagus. Also, it is important to take out lymph glands that lie alongside the oesophagus and stomach because cancer cells may have spread to these glands. This is called lymphadenectomy. This operation involves surgical work in your abdomen (tummy) and in the right side of your chest. Your stomach is made into a tube that is taken up into your chest and joined to the cut end of your oesophagus.
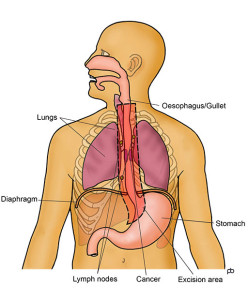
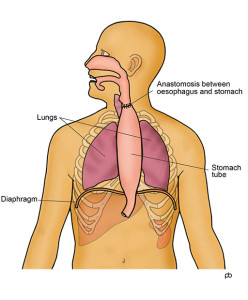
The McKeown operation is done for tumours in the middle part of the oesophagus. In this operation, the entire oesophagus is removed. Like the Ivor Lewis operation, surgical work is done in your abdomen (tummy) and in the right side of your chest. In addition, a cut is made in the left side of your neck. The oesophagus is divided in the neck, a short distance below your voicebox. The stomach is made into a tube that is brought up in to your neck and joined to the cut end of your oesophagus.
The surgical work in your abdomen or chest or both can be done by keyhole surgery (laparoscopy). This is called Minimally Invasive Oesophagectomy (MIO). The decision about the type of operation and whether to do the operation through large cuts or keyholes depends on your individual circumstances.
What is the risk that cancer of the oesophagus can come back after an operation?
The risk that the cancer will come back (called recurrence of cancer) depends mainly on the final pathological stage of the cancer. The oesophagus and surrounding gland glands that are removed by surgery are examined in the detail in the pathology laboratory. The final stage takes various features of the cancer into account. How deep does the tumour go into the wall of oesophagus (T stage)? How many lymph glands are involved by cancer (N stage)? How close that the cancer go to the margin? Cancers at an early stage have better prognosis than advanced cancers. The prognosis is often stated as 5-year survival. This means the number of patients with that stage of cancer who will be alive after 5 years.
It is more difficult to estimate the prognosis before treatment has started. Staging tests are not always accurate. Sometimes, pathology may show that the tumour is more advanced than was shown by the pre-operative tests. Also, prognosis depends on your general fitness, response to chemotherapy and recovery from the operation. We can make estimates about prognosis based on your individual circumstances, but we cannot be certain.